How Clean Are Your Disposable Gloves?
Infection control management systems play a critical role in healthcare and food sectors, helping to minimise the risk of cross-contamination and pathogen infection. It is reported that in Aotearoa, New Zealand, 10% of inpatients develop a hospital-acquired infection, annually costing hospitals between $50 and $85 million. It is also estimated that food-borne illnesses cause nearly 200,000 people to be sick annually.
Glove cross-contamination is a global issue and has been implicated as a contributory cause in over 15% of (food-borne) outbreaks investigated.
New and unused disposable gloves should be clean; you shouldn’t expect anything less! However, scientific studies have found a large variety of bacterial contamination on new and unused single-use gloves, including pathogens responsible for food-borne illnesses (FBIs), human skin bacteria and other pathogenic contaminants.
GLOVE CONTAMINATION STARTS AT THE FACTORY
Have you considered that bacteria, such as Staphylococcus aureus and E. coli, can grow in unused glove boxes due to a lack of optimal factory hygiene during the glove manufacturing process?
Glove production is largely unregulated, and FDA compliance for food handling or medical use does not include testing for microbial contamination or bioburden.
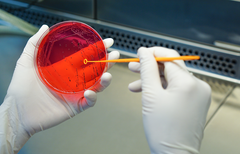
Testing of new, unused gloves, by Eagle Protect, in collaboration with internationally recognised microbiologist Barry Michaels, has further confirmed the presence of pathogens and microbes responsible for FBIs (including E. coli and Staphylococcus), as well as microbes linked to food spoilage and occupational skin disease. These contaminants originate from:
- Polluted surface water from agricultural, industrial and urban run-off
- Wastewater, human faeces and animal gut bacteria
- Factory water filtration units
- Glove drying cycles
- Human skin bacteria
- Paperboard packaging
Hazards can be created when manufacturers attempt to cut costs. These shortcuts can introduce both microbial and chemical contamination while also reducing glove durability.
The video below highlights the critical control points (CCPs) in the manufacturing process—areas where inadequate hygiene, contaminated water, subpar materials, insufficient leaching, improper drying, and unhygienic packaging can all facilitate the development of contamination.
WHY IS THIS BECOMING AN ISSUE?
For operations with Organic Certification or microbial testing requirements, gloves must be clean, non-toxic, and free from harmful pathogens.
One of the most common shortcuts in low-cost glove manufacturing is reducing wash-tank clean-outs or using lower-quality water, which allows microbes and chemicals to accumulate. This can have serious consequences for food safety and worker health.
Study Findings On Unused Protective Gloves
Research shows:

- Environmental contaminants of up to 10,000 bacteria per glove
- Skin commensals of up to 1,000 CFU per glove
- Bacteria can continue to grow inside packaged, non-sterile gloves
A well-regarded New Zealand hospital study found:
- 81.6% of disposable gloves were contaminated with environmental bacteria
- 50% contained skin commensals
- Contamination was present in boxes opened on day 0, indicating transfer during manufacturing
- Over 80% of the gloves were contaminated immediately upon opening
This may not be of danger, but the most likely implication of the sanitary conditions (or lack thereof) in the offshore glove production and packing facility. While a certain amount of environmental bacteria is inevitable in the manufacturing process, an effort should be made to keep levels to a minimum because they are an infection risk, especially for people who are immunocompromised.
ENSURING CLEAN GLOVES
Reliable and consistent glove sourcing is essential to stop the spread of pathogens to food and other contact surfaces.
Eagle Protect nitrile gloves are rigorously tested for bacterial contamination:
-
Total bacterial count = 0 immediately after production, after 6 months, and after 1 year of ageing
Steve Ardagh, CEO of Eagle Protect, explains:
“Our factories have significant systems in place to both prevent this sort of bacterial contamination and tests to ensure this is the case.
There are extra-length cleaning tanks which are used to leach out any chemicals left after the dipping and drying process. Gloves are stripped off the Formers by hand and then placed in bags immediately and double sealed. They are moved to the packaging areas as needed for sales in positive airflow controlled environments."
Help stop the spread of cross-contamination. Choose a reliable glove supplier with rigorous quality control testing and manufacturing standards in place. Let us help safeguard what matters most to you.
REFERENCES:
- Michaels, B 2018. Determination of the % of Food-borne Outbreaks (FBIs) Attributed to Glove-Related Cross-Contamination Causes.
- Cornwall J, Hughes K, Theis J-C, Brooks H. 2006. Bacterial Contamination of Unused, Disposable Non-Sterile Gloves on a Hospital Orthopaedic Ward. Am. J. Infect. Cont. 34(3):128-30.
- Ferreira AM, de Andrade D, Haas VJ. 2011. Bacterial contamination of non-sterile disposable gloves before use. Rev. esc. enferm. USP. 45(3).
- Hughes KA, Cornwall J, Theis JC, Brooks HJ. 2013. Bacterial contamination of unused, disposable non-sterile gloves on a hospital orthopaedic ward. Australas Med J. 2013 Jun 30;6(6):331-8.
- Kramer A, Assadian O. 2016. Indications and the requirements for single-use medical gloves. GMS Hyg Infect Control. 2016; 11: Doc01.


